It can be incredibly frustrating when your health insurance provider denies coverage for a medical service or treatment that your doctor insists is absolutely necessary. You’ve followed all the rules, received professional medical advice, and yet you find yourself facing an unexpected bill or being told a vital procedure won’t be covered. This situation is unfortunately common, but it’s important to remember that a denial isn’t always the final word. You have the right to appeal these decisions.
Navigating the complexities of insurance appeals can feel overwhelming, especially when you’re already dealing with health concerns. That’s why having a solid framework, like an appeal letter template for medical necessity, can make a huge difference. This guide is designed to help you understand the appeal process and equip you with the knowledge to craft a compelling letter that clearly articulates why your denied service is, in fact, medically essential.
Understanding Why Your Claim Was Denied
Before you can effectively appeal a denial, it is crucial to understand *why* your claim was rejected in the first place. Insurance companies are required to send you an Explanation of Benefits EOB or a denial letter outlining the specific reasons for their decision. Don’t just glance at this letter and get discouraged; it contains vital information that will inform your appeal strategy. Take the time to read it carefully, looking for policy numbers, claim numbers, dates of service, and the exact code or language used to justify the denial.
Often, denials for medical necessity stem from the insurer’s interpretation of their policy, a lack of specific documentation from your healthcare provider, or simply a bureaucratic error. It is not uncommon for insurance companies to label a treatment as “experimental,” “investigational,” or “not medically necessary” even when your doctor strongly believes it is the most appropriate course of action for your condition. Your job in the appeal is to counter these claims with clear, evidence-based arguments.
Common Reasons for Medical Necessity Denials
Once you have identified the precise reason for the denial, you can begin gathering the appropriate information and evidence to support your position. This often means working closely with your healthcare provider’s office to ensure all clinical notes, test results, and letters of medical necessity are complete, accurate, and directly address the insurer’s concerns. Remember, the more comprehensive and persuasive your documentation, the stronger your appeal will be.
Crafting Your Effective Appeal Letter
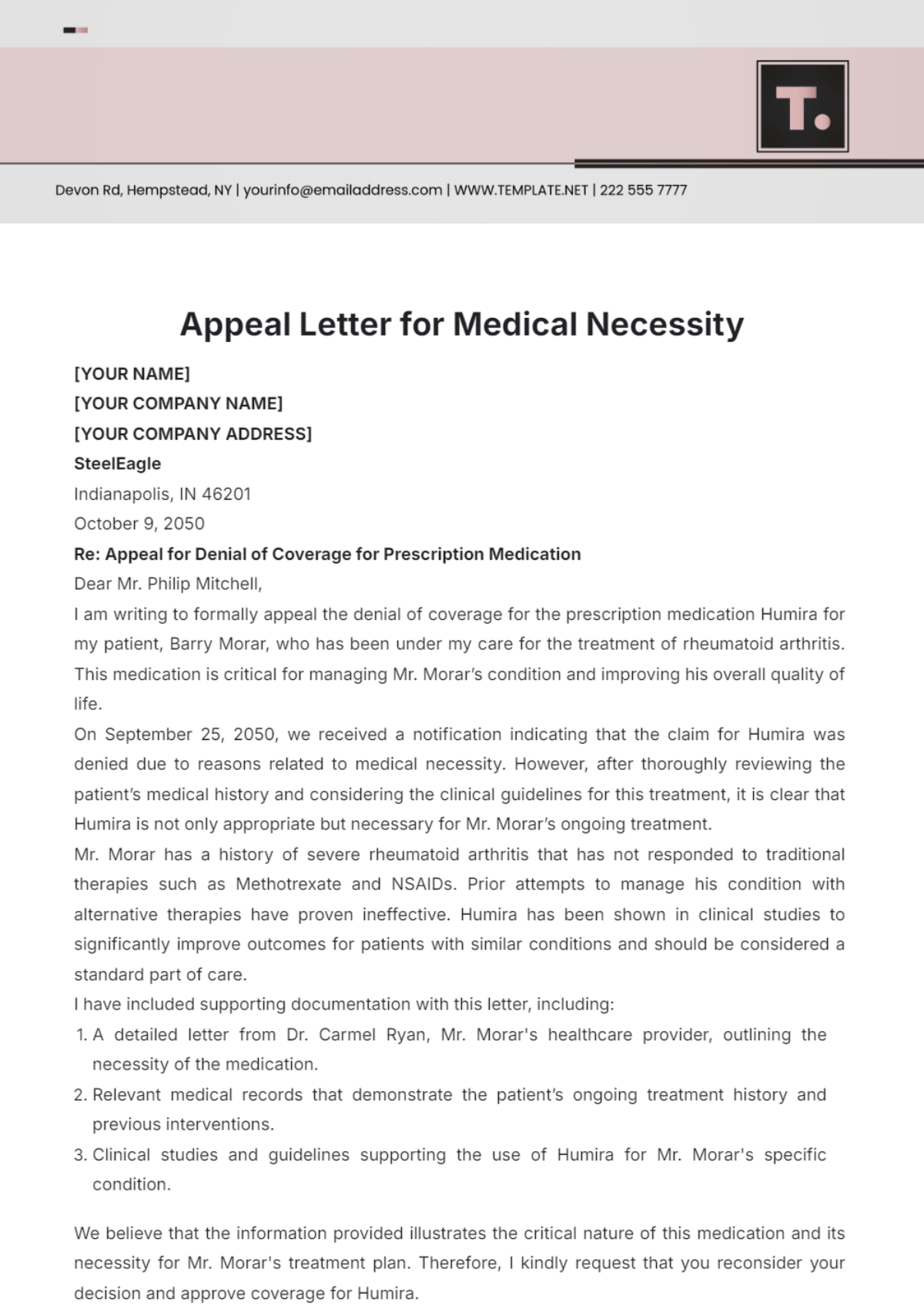
Writing an appeal letter can seem daunting, but it’s essentially a formal request for your insurance company to reconsider their decision. Your goal is to present a clear, concise, and compelling argument supported by medical evidence. The letter should be professional in tone, yet firm, emphasizing that the denied service is crucial for your health and well-being. Think of it as building a robust case that leaves little room for doubt regarding the medical necessity of your treatment.
Start by clearly stating your intent to appeal and include all identifying information for yourself and the claim in question. This ensures your letter is correctly routed and reviewed promptly. Be sure to reference the specific denial letter you received, including its date and claim number. Then, get straight to the point: explain what service was denied and why you believe it is medically necessary, directly addressing the reason for denial as stated by your insurer.
It is absolutely vital to include supporting documentation with your letter. This can include a detailed letter from your doctor outlining your diagnosis, the treatment plan, why this specific treatment is necessary, and what the potential negative outcomes might be if it is not received. Clinical notes, relevant test results, and even peer-reviewed medical literature supporting the efficacy of the treatment can significantly bolster your case. The more evidence you provide that aligns with your doctor’s recommendation, the better your chances of a favorable outcome.
When you use an appeal letter template for medical necessity, make sure to customize it thoroughly with your specific details and medical information. While a template provides structure, the personalization is what truly makes your appeal compelling. Conclude your letter with a clear request for reconsideration and provide your contact information, along with a reasonable timeframe for a response. Always keep a copy of everything you send, including your letter and all attachments, for your records. Consider sending your appeal via certified mail with a return receipt requested, providing proof of delivery.
Navigating a medical necessity denial requires persistence and careful attention to detail, but you are not alone in this process. By understanding the reasons behind a denial and meticulously preparing your appeal, you significantly increase your chances of overturning the original decision. Your health and access to necessary medical care are paramount, and taking these steps demonstrates your commitment to receiving the treatment you deserve.